The Male Infertility Problem[1]
Infertility is the inability to conceive after 12 months of regular, unprotected intercourse. This reproductive health problem affects more than 15% of all reproductive-aged couples worldwide. What is rarely recognized is that male infertility contributes to more than half of all of these cases. Male infertility involves four major categories of sperm defects, any one of which leads to a diagnosis of male infertility. These include low sperm count (oligozoospermia), poor sperm motility (asthenozoospermia), defects of sperm morphology (teratozoospermia), and total absence of sperm in the ejaculate (azoospermia). Azoospermia may be due to lack of sperm production (non-obstructive azoospermia) or blockages in sperm transport (obstructive azoospermia). These four types of male infertility account for about 40% of all cases of infertility in Western countries. However, in the Middle East, 60–90% of all cases presenting to in vitro fertilization (IVF) centers involve a diagnosis of male infertility, according to physician estimates. Moreover, non-obstructive azoospermia is highly prevalent in the Middle East, as are cases of severe oligoasthenozoospermia (i.e., very low sperm count and poor motility). Because of advances in the field of genetics, it is now known that a significant percentage of these kinds of severe cases are due to genetic abnormalities. In the Middle East, severe cases of male infertility tend to run in families, and are probably related to intergenerational patterns of consanguineous (cousin) marriage, which increase the chances for genetic mutations, including microdeletions of the Y chromosome linked to male infertility.
In short, male infertility is especially common in the Middle East and quite common elsewhere, but this is not popularly known. Male infertility has been called a “neglected” reproductive health problem, and one that remains deeply hidden, including in the West. Studies in the United States have shown male infertility to be among the most stigmatizing of all male health conditions. The depth of this stigmatization may be even deeper in non-Western settings such as the Middle East, casting a permanent shadow on a man’s community standing. Such stigmatization is clearly related to issues of sexuality. Male infertility is popularly, although usually mistakenly, conflated with impotency (i.e., erectile dysfunction), as both disrupt a man’s ability to impregnate a woman and to prove one’s virility, paternity, and manhood. This “fertility-virility linkage” means that men who are infertile are assumed to be impotent, even though most are not. Furthermore, because male infertility tends to be deeply hidden, Middle Eastern women tend to bear responsibility — even if misattributed — for failures of reproduction.
The ICSI Solution
Because male infertility is often related to genetic defects of sperm production, it is recalcitrant to prevention, and among the most difficult forms of infertility to treat. Male infertility is generally not a condition that can be “cured” per se. Instead, it represents a chronic reproductive health condition for millions of men worldwide.
In the Middle East, the advent of laboratory-based semen analysis did not become widespread until the 1970s, nor did it become fully reliable according to World Health Organization standards until much later. Furthermore, until the early 1990s in the West, the only known solution to male infertility was donor insemination (DI), the oldest of the reproductive technologies, but one that is religiously prohibited across most of the Muslim world. The introduction of intracytoplasmic sperm injection (ICSI) — pronounced “ick-see” — in Belgium in 1992 was a watershed event. A variant of IVF, ICSI solves the problem of male infertility in a way that IVF cannot. With standard IVF, spermatozoa are removed from a man’s body through masturbation, and oocytes are surgically removed from a woman’s ovaries following hormonal stimulation. Once these male and female gametes are retrieved, they are introduced to each other in a petri dish in an IVF laboratory, in the hopes of fertilization. However, “weak” sperm (i.e., low numbers, poor movement, misshapen) are poor fertilizers. Through “micromanipulation” of otherwise infertile sperm under a high-powered microscope, they can be injected directly into human oocytes, effectively “aiding” fertilization (Figure 1). As long as one viable spermatozoon can be extracted from an infertile man’s body, it can be “ICSI-injected” into an oocyte, leading to the potential creation of a human embryo. With ICSI, then, otherwise “sterile” men can father biogenetic offspring. This includes azoospermic men, who produce no sperm in their ejaculate and must therefore have their testicles painfully aspirated or biopsied in the search for sperm. In short, ICSI gives infertile men a greater chance of producing a “take-home baby.”
Figure 1: Intracytoplasmic Sperm Injection (ICSI)
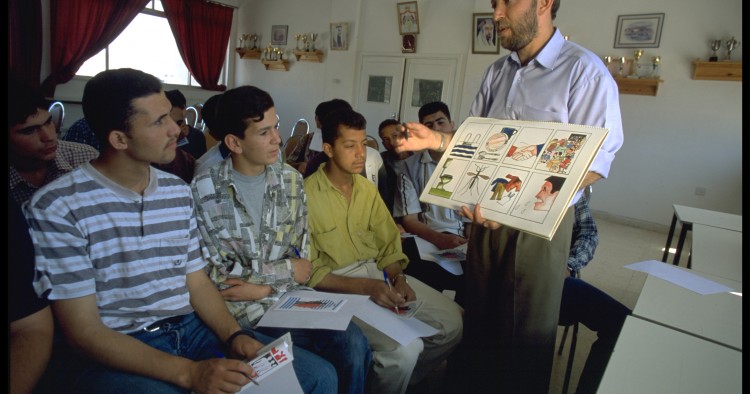
The coming of ICSI to the Middle East in 1994, where it was introduced in an IVF clinic in Cairo, has led to a virtual “coming out” of male infertility across the region, as men acknowledge their infertility and seek the ICSI solution. The coming of this new “hope technology” has repaired diminished masculinity in men who were once silently suffering from their infertility. Furthermore, ICSI is being used in the Middle East and elsewhere as the assisted reproductive technology “of choice,” effectively replacing its predecessor IVF. Basically, IVF leaves fertilization “up to chance,” whereas ICSI does not. Thus, ICSI provides a more guaranteed way of creating “the elusive embryo.” With ICSI, human fertilization is increasingly aided and abetted by human embryologists working in IVF laboratories around the world.
Figure 2: ICSI Being Performed by an Embryologist in Beirut, Lebanon
ICSI may be a “breakthrough” technology, but it is by no means a panacea. For one thing, the precisely timed collection of semen can produce deep anxiety and even impotence, but is imperative for all ICSI procedures. Second, some men produce no spermatozoa whatsoever, eliminating ICSI as an option. Third, ICSI sometimes does not succeed, leading to endless rounds of fruitless repetition among some couples. Fourth, ICSI involves a grueling surgical procedure for women as it is highly dependent upon the complicated stimulation and extraction of healthy oocytes from women’s bodies. Whereas the fecundity of older men can often be enhanced through ICSI, women’s fertility is highly age sensitive, with oocyte quality declining at later stages of the reproductive life cycle. In short, older women may “age out” of ICSI, causing highly gendered, life-course disruptions surrounding women’s “biological clocks.” Fifth, men may “arrive” at ICSI after years of other failed treatment options. ICSI is expensive, usually costing $2,000-6,000 per cycle in the Middle East. Thus, it is often deemed a “last resort,” especially for men without adequate financial resources. Finally, when it does succeed, ICSI may be perpetuating genetic defects into future generations, through mutations of the Y chromosome and other inherited disorders that may be passed by ICSI to male offspring. The ethics of passing genetic mutations to children has been an increasing cause for concern.
Recent research suggests that male reproductive tract abnormalities — including undescended testicles, hypospadias (a birth defect in which the opening of the urethra is on the underside, rather than at the end, of the penis), and poor semen quality — are more prevalent in male children conceived through assisted reproduction, regardless of genetic defects in their fathers’ sperm. This is because assisted reproduction is associated with the use of artificial hormones, higher rates of prematurity, low birthweight, and multiple gestation, which are indirect risk factors for the development of male genital malformations (from the disruption of gonadal development during fetal life). ICSI, in particular, increases the risk for hypospadias, which may require surgical repair during infancy.
Despite these challenges, nearly 5 million “test-tube babies” have now been born around the world, nearly half-a-million of whom are the result of ICSI. ICSI is a “hope technology,” creating the “only hope” for most infertile men, especially those with serious cases. The emergence of ICSI in the Middle Eastern region in the mid-1990s led to an immediate boom in demand for this technology — a demand that has never waned. IVF clinics today are filled with ICSI-seeking couples. ICSI is by far the most common assisted reproductive technology now undertaken in the Middle East. As one infertile Lebanese man put it, “I will try again and again and again. I will never lose hope.” Or, as another concluded, “I will try until I die.”
[1]. Material for this article is excerpted from the author’s new book, The New Arab Man: Emergent Masculinities, Technologies, and Islam in the Middle East, to be released by Princeton University Press in March 2012.
The Middle East Institute (MEI) is an independent, non-partisan, non-for-profit, educational organization. It does not engage in advocacy and its scholars’ opinions are their own. MEI welcomes financial donations, but retains sole editorial control over its work and its publications reflect only the authors’ views. For a listing of MEI donors, please click here.